After decades of efforts by advocates fighting in the trenches of America’s ongoing opioid crisis, harm reduction is finally having its day. Late last month, New York City opened the doors of its first supervised injection sites, or overdose prevention centers—the first such facilities in the nation. On day one, the staff saved two people’s lives.
It’s taken a long time for supervised injection sites to open, mainly because they operate in a legal gray area. But overdose deaths have reached record levels because fentanyl, a painkiller 50 times more potent than heroin, is increasingly being laced into heroin supplies and putting users at unprecedented risk of overdosing. The fallout of the Covid-19 pandemic hasn’t helped: In 2021, a record-breaking 100,0000 people have died from drug overdoses in the United States.
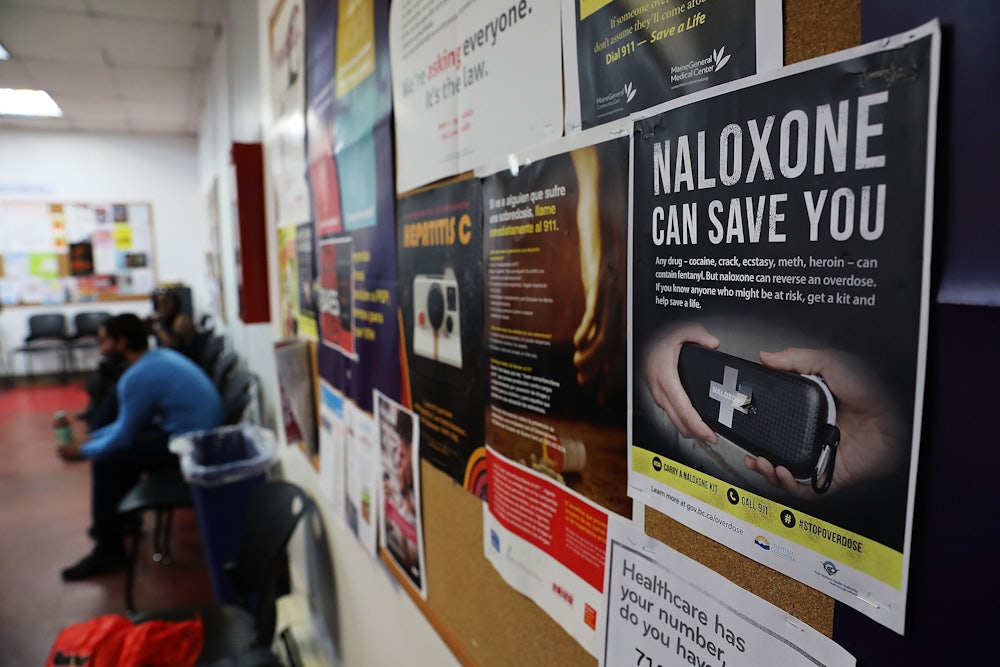
Overdose prevention centers give participants a safe place to use, under supervision of medical staff who have clean needles and naloxone on hand, as well as equipment to test drugs for fentanyl. These centers also provide resources for health and social services, including treatment for substance use disorders.
Harm reduction “used to be a totally taboo subject,” according to Maritza Perez, director of the Office of National Affairs at the Drug Policy Alliance. Now, she says, more people are recognizing that harm reduction “actually meets people where they are at and [does] work to save lives and ultimately hopefully connect people to health services.”
Joe Biden has become the first U.S. president to speak publicly in favor of harm reduction, after decades of failed enforcement policies that purport to police their way out of a public health issue. Last week, the Substance Abuse and Mental Health Services Administration announced the first round of federal grants for harm-reduction programs. There are efforts on the Hill to make it easier to access drug treatment, which the Biden administration has already made some effort to relax. However, the administration stopped short of explicitly endorsing the overdose prevention centers.
“It’s a promising time,” said Dr. Bruce Trigg, a longtime harm-reduction and addiction medicine doctor who works with the Bronx-based St. Ann’s Corner of Harm Reduction. “But the crisis is worse than it’s ever been.” Since Thanksgiving, two patients at his facility have overdosed.
The depth of the opioid epidemic—and the graveyard of overdose deaths it has produced—has forced the administration to admit that the status quo doesn’t work. Even tepid acknowledgments that there might be something to harm reduction is a huge step. But it’s only a small part of the effort to shift drug policy from the purview of the criminal justice system into the public health sphere.
In order to take a larger step toward solving the overdose crisis, we must face the failures of our health care system. People at higher risk of developing an opioid use disorder—including those with chronic physical and mental health conditions and trauma, uninsured people, and low-income communities of color—face barriers to life-saving comprehensive medical care. Legal restrictions add further barriers, subjecting those with opioid use disorder to a dizzying, fragmented maze of coverage plans and regulations. The opioid epidemic can’t be fully overcome without a new approach to our privatized insurance and health care system.
Our current system makes it extremely difficult to access effective treatment. While nearly two million people report having an opioid use disorder in the U.S., less than 10 percent of those who need treatment are receiving it. Although a 2008 law that sought to require most insurance plans to include substance use and mental health treatment was strengthened by the Affordable Care Act and Medicaid expansion, the definition and application of that treatment has varied widely in practice. Notwithstanding the millions of people without insurance, those with Medicaid or private insurance face a daunting patchwork of networks, authorizations, and requirements to access covered care.
The use of evidence-backed medications, particularly methadone and buprenorphine (brand name Suboxone), to treat opioid dependence is a vital tool in the fight. Most state insurance plans cover buprenorphine and naltrexone, but just over half cover methadone, according to a trove of data from the Prescription Drug Abuse Policy System. Less than two-thirds also include coverage for behavioral health services related to opioid use disorder. (The majority of private rehab centers don’t use medication.)
Those with private plans are by no means better off. Only eight states require commercial insurance to cover medication-based treatment for opioid use disorder. And about a fifth of adults with an opioid use disorder are uninsured, making them particularly vulnerable to overdose and death.
Moreover, private insurance coverage restrictions differ from state to state and plan to plan, forcing doctors and billing staff to dedicate massive amounts of time to determine who and what is in-network and who and what is out. Participants are limited by age, number of refills, quantity of pills, and cost caps and are usually subject to prior authorization requirements. Some insurance companies will only cover certain clinics or only portions of the costs. Trigg called the requirements “complete nonevidenced bullshit.”
Methadone, which has been highly successful in helping people stop heroin, can only be dispensed at specialized clinics and often requires people under its treatment to spend hours every day for dosing and supervision, explained Trigg. That burden is such that two of Trigg’s patients dropped out of their methadone programs during Covid-19. “They had children and jobs, and couldn’t go every day,” he said. Both have since relapsed.
“The system used to look for excuses not to treat people. Now we should be bending over backward to get anyone into treatment who wants it,” said Trigg.
Buprenorphine, for its part, may be more promising in providing low-threshold treatment to patients. It’s safer than methadone because it’s nearly impossible to overdose on, and some patients prefer it because it’s less sedating and less disruptive to life. It can be prescribed in a primary care setting by any prescribing health professional with the appropriate waiver. Getting that waiver used to require doctors to attend an eight-hour training, but that requirement has been dropped in a bid to get more doctors to agree to treat people with opioid use disorders, explained Dr. Daniel Alford, a primary care physician and director of the Safe and Competent Opioid Prescribing Education, or SCOPE of Pain, program at the Boston University School of Medicine.
Still, just 7 percent of primary care providers have that waiver. Due to the stigma that people with addiction are untrustworthy, volatile patients, many doctors don’t want the responsibility. But for Alford, prescribing buprenorphine is one of his most rewarding experiences as a doctor. “People with opioid use disorder who you start on buprenorphine, oh my God,” he said. “They’re no longer in withdrawal, they’re able to focus on other things, I mean, it’s just remarkable.”
Unfortunately, access to buprenorphine is often segregated along racial lines. Studies have shown that Black and Latinx communities have more facilities that provide methadone per capita, while white communities have more access to buprenorphine, the newer and less disruptive medication treatment option. “The same disparities that you see in the health care system are prevalent when we’re talking about people with substance use disorder,” said Perez.
In addition to medication-assisted drug treatment, the widespread use of naloxone, the overdose-reversing drug, is key to ending opioid overdoses. But as demand for naloxone has skyrocketed, so has price gouging from pharmaceutical companies. While you used to be able to get a dose of Narcan for $2.50, it can now cost up to $75 or more. And while Purdue got a slap on the wrist for its role in starting the opioid crisis, its malfeasance has continued: Beyond price gouging naloxone, it also marketed fentanyl in the parts of the country hardest hit by the crisis.
“The pharmaceutical industry has total control,” said Trigg, who is also a board member with the Physicians for a National Health Program. “As a result, we either have to give out less naloxone, or health departments and public agencies that pay for it have to cut back on other things.”
The rampant profiteering and fragmentation of care isn’t limited to drug treatment. The lack of comprehensive, affordable, and quality mental and physical health services has also spurred addiction, especially among groups who are most at risk of developing an opioid use disorder—uninsured people, those with mental health conditions and/or past trauma, and people suffering from chronic pain.
Research has shown that mental health conditions and substance use disorders are often comorbid: Up to half of those who have a mental illness in their lives will also experience an addiction, according to the National Institute on Drug Abuse. Despite the law that mental health and drug treatment must be covered by insurance, networks are limited, and behavioral health specialists, especially those who are able to prescribe medication, are often not taking new patients.
A 2019 study by the National Alliance for Mental Health showed that behavioral health visits are five times more likely to be out of network than an appointment with a primary care provider. These inadequate networks “effectively discriminate” against people needing this care, concluded the report.
Trigg said that he’s had so much trouble finding a psychiatrist for his patients, even though they all have Medicare, that he’s resorted to prescribing them antidepressants himself, even though it’s outside his specialty. Many of his patients have also had bad experiences with mental health professionals who treat them with scorn and mistrust.
The role of trauma in fueling addiction is another reason why access to affordable behavioral health care is so important. As addiction researcher Gabor Maté put it in a recent article in Yes! magazine: “We have a social structure that induces trauma in a lot of people. Therefore, it induces escapist, addictive behaviors.” And when accessing health care adds to that trauma rather than addressing it, it makes people less likely to pursue it in the future.
The lack of coordination between mental and physical health care and the fragmentation of our system contribute to the cycle of self-medication. As Trigg posited: “How many people have a primary care provider who they can talk to, who asks about depression and substance use?”
Among those who do have a doctor, few feel comfortable talking about their drug use. Alford said that some doctors he’s worked with to train them on appropriate prescribing practices for opioids have gone so far as to “fire” their patients when they’ve tested positive for drugs. This, of course, is a time when those patients need care more than ever.
“Many people may not feel comfortable going to a medical provider because they might face criminal repercussions or discrimination, and we know that that typically happens to Black and brown people,” said Perez.
Alford led a 2016 study that found that a whopping 87 percent who tested positive for drugs or heavy alcohol use had chronic pain. And 81 percent of those who misused a prescription drug did so to self-medicate. The 2019 National Survey on Drug Use and Health reported that two-thirds of people who last abused a prescription were also trying to relieve pain. The majority got the drugs from a family member or friend—just 7 percent bought them off the street.
These figures “speak to the complexity of managing chronic pain and also the lengths that people will go to relieve that suffering,” said Alford.
For patients without a trusting relationship with a primary care doctor who helps coordinate their care, it can be much easier for a provider to prescribe painkillers than to look comprehensively at the root of preexisting health problems that cause pain. (It’s important to note that opioids do have legitimate medical uses. “There is no question that there are patients who are more functional because they’re able to get this one type of medication, and they’re taking it as prescribed, and they’re doing just fine,” says Alford.)
There are other treatments for pain, pharmacological and otherwise, that can help people manage their symptoms. Many of these—such as cognitive behavioral therapy, massage therapy, acupuncture, lidocaine injections, and nerve blocks—are often not covered by insurance. Moreover, new medications can be exorbitantly expensive; insurance companies often refuse to cover them.
It’s no surprise, then, that many have plunged into medical debt, which only exacerbates the impact of opioid use disorders among the same at-risk groups: low-income individuals, the uninsured, and people with chronic medical conditions, according to the Kaiser Family Foundation.
Doctors can’t help their patients when they’re spending a prodigious amount of time fighting with insurance providers. According to a 2018 doctors’ survey, nearly a third of doctors reported spending 20 hours or more a week on paperwork. It’s well documented that patients who spend more time with their doctors have better health outcomes, but our health care system incentivizes doctors to see as many patients as they can as quickly as possible and then turn to the giant stack of prior authorizations on their desks.
In short, there is no way to address the opioid crisis—both in terms of treating people with opioid use disorder as well as caring for people who could develop it—without massive reforms. A good first step would be the creation of a national formulary for pharmaceuticals, which would enshrine one set of rules that could apply to everyone, freeing doctors and staff from having to comprehend the intricacies of each individual plan’s coverage. Biden recently introduced a prescription drug–pricing framework as part of the Build Back Better bill, which, if passed, would help address big pharma’s profiteering of life-saving medications.
Harm reduction is an important step in the right direction of shifting our drug policy from a criminal justice to a public health lens. But acknowledging that drug users deserve not to die is really only the barest of minimums. We need to go further to meet the scale of the crisis, through a single-payer system that would take profit out of the health care system entirely. Given the scale of the crisis, any harm-reduction policy must prioritize making mental and physical health services, including treatment, accessible to all.
“The pivot to harm reduction in both Congress and the administration is fantastic, but it’s not enough,” said Perez. “We need to use every tool at our disposal, and go big.”